Short answer: CBD can help restore good bacteria after antibiotics by interacting with the ECS (endocannabinoid system) and certain gut flora. CBD is one of several methods for restoring good bacteria.
In 2019, there were over 100 antibiotics that fell into seven main classes. Pharmaceutical companies design different antibiotics and combinations to fight infections in specific areas of the body.
Certain drug-resistant bacteria require a large list of antibiotics required to handle the more dangerous bacteria. Even with a large mix of antibiotics, some of these “super-bugs” are not being dealt with – effectively.
Recent research is revealing evidence of a plant-based antibacterial activity found in hemp. Plant-based antibacterials have certain molecules called cannabinoids, such as CBD.
Cannabinoids are showing potent activity towards several strains of multidrug-resistant bacteria, such as MRSA (methicillin-resistant Staphylococcus aureus). According to research, MRSA is taking more lives than AIDS. Since cannabinoids show a powerful interaction with drug-resistant bacteria, identifying specific targeting mechanisms remains elusive.
Where to purchase quality broad-spectrum cannabinoid + CBD oil – with zero THC?
There are only a few CBD brands on the market that are of quality and legal for Idaho markets.
CBD Vs Antibiotics: How Do You Replace Good Bacteria After Antibiotics Destroy Them?
Understanding how to replace the good bacteria after antibiotics destroy them requires us to answer a few fundamental questions:
- What are antibiotics?
- How do antibiotics actually work?
- Do antibiotics kill good bacteria in the body?
- What are the potential side effects of antibiotics?
- Are antibiotics bad or harmful?
- How do you replace good bacteria after antibiotics destroy them?
What are antibiotics?
Antibiotic means against life and the first true antibiotic was called penicillin – discovered in 1928 by Alexander Fleming.
They are a type of drug – or antimicrobial – targeting infections triggered by bacteria.
Antibiotics differ from antiseptics, where an antiseptic sterilizes the surface of living tissue (skin). Disinfectants are another type of antimicrobial used to kill micro-organisms (bacteria) on non-living surfaces.
Other types of (harmful) bacteria include fungi and viruses.
All drugs designed to kill germs in the human body are considered an antibiotic.
Any substance (material) that obstructs the growth, prevents reproduction, or all out kills the bacterium is technically an antibiotic. How antibiotics work is one of three basic methods.
The three basic ways antibiotics work are:
- Killing bacteria.
- Keeping bacteria from reproducing.
- Slowing bacteria from growing.
After antibiotics started getting widely used, in 1940, the first penicillin-resistant infection evolved caused by the bacterium Staphylococcus aureus. Staph infections can infect several areas of the body.
How do antibiotics actually work – technically?
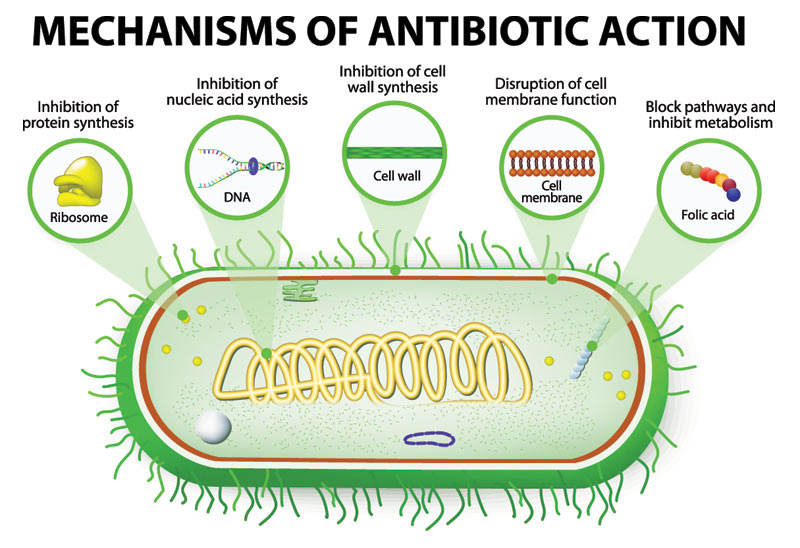
What causes antibiotics to seek bacterial cells without interacting with human cells involves a handful of processes.
There are certain similarities and differences between human and bacterial cells. How antibiotics actually work involves targeting things bacterial cells have that human cells do not have.
How do antibiotics actually work is by:
- Preventing bacteria from building a cell wall (human cells don’t have cell walls).
- Dissolving bacterial cells membrane and not human cell membranes.
- Affecting bacterial protein-building.
- Interfering with the bacterial cells DNA-copying machinery.
Different antibiotics are designed to target infections in specific areas of the body. Different combinations of antibiotics may be required to kill certain bacteria.
Do antibiotics kill good bacteria in the body?
One drawback of antibiotics is that they kill good bacteria along with the necessary bad bacteria inside a person. Good bacteria is designed to keep you healthy in several ways.
Taking antibiotics can cause your health to suffer and may create room for the bad bacteria to multiply – leading to potential multiple infections.
Overusing antibiotics is bad and can have severe side effects. Over larger amounts of time, taking antibiotics can make bacteria that are harder to kill.
Harder-to-kill bacteria are known as antibiotic resistance.
What are the potential side effects of antibiotics?
What are the most common side effects of antibiotics that typically target the digestive system? The most common side effects of antibiotics affect approximately 1 in 10 people.
Common side effects of antibiotics are:
- Vomiting.
- Nausea.
- Diarrhea.
- Bloating.
- Indigestion.
- Abdominal pain.
- Loss of appetite.
- And potentially more.
Allergic reactions are also possible with antibiotics. Common allergic reactions range from mild to modern including; itchy skin rash, coughing, wheezing, tight throat, and more.
More uncommon severe allergic reactions to antibiotics can be life-threatening and cause anaphylaxis. Anaphylaxis symptoms peak in severity within 5 – 30 minutes and involve rapid heartbeat, difficulty breathing, a sudden drop in blood pressure, unconsciousness, and more.
Antibiotic side effects can last up to two weeks after you’ve taken your last dose.
Are antibiotics bad or harmful?
Some types of infections begin when the antibiotic kills too many friendly bacteria and allows the bad bacteria to infect.
When antibiotics kill too many good bacteria, certain bad bacteria multiply and produce toxins – making you sick. Symptoms of antibiotic damage include fever, nausea, diarrhea, and inflammation.
The only way to prevent antibiotics from damaging good bacteria is to not take antibiotics too frequently and only taking antibiotics when it’s absolutely necessary.
Antibiotics are not able to kill viruses, the flu, or any other common cold. Taking an antibiotic when you have a virus may cause more harm.
To prevent overusing antibiotics, it’s best to only take an antibiotic if you need it. Taking antibiotics when you don’t really need them causes bacteria to grow stronger and resist antibiotics.
How do you replace your body’s good bacteria after antibiotics destroy both good & bad bacteria?
How to replace good bacteria after antibiotics includes a handful of options to help restore your gut flora and rebuild your army of good bacteria.
Since antibiotics are well known to kill any type of bacteria (good or bad), the strategy is to not take an antibiotic – every time you think you might need to.
In the early days of medicine, doctors thought healthy bodies were sterile bodies and the immune system is always at war with microscopic organisms you interact with – daily.
As the medical industry continues to gather new information, an entirely new world filled with good types of living microscopic creatures are what continues to maintain health. Having a proper balance of healthy bacteria in your intestines and other areas of your digestive tract helps.
Good bacteria help by digesting and absorbing food nutrients and fighting back bacteria that could make you sick.
How do you replace bacteria after antibiotics include:
- Broad-spectrum CBD oil (cannabidiol).
- Taking prebiotics & probiotics (good bacteria).
- Cut out sugar (various bacteria thrive on sugar).
- Sip on bone broth.
- Eat lots of fruits & vegetables.
- Low animal fats & products.
- Juice fresh fruits (Juice Recipe: Boost Gut Health)
- Exercise.
- Reduce stress.
Recent research is showing evidence of antibacterial activity in a wide range of cannabinoids – found in the hemp plant. Cannabinoids listed as having antibacterial properties are CBD (cannabidiol), CBC (cannabichromene), CBG (cannabigerol), and more.
New antibacterials, such as broad-spectrum cannabinoid oil, are needed due to the growing challenges current doctors face with MDR (multidrug-resistant) bacteria. A recent extreme MDR bacteria emerged known as XDR-TB (mycobacterium tuberculosis).
Extreme drug-resistant bacteria are emerging and making current antibiotics somewhat ineffective. In the last 30 years, only one new class of antibacterial drugs has been added to modern medicine.
Despite the knowledge that many plants having powerful abilities to handle drug-resistant bacteria, fully utilizing plants and known antibacterial (full-spectrum) cannabinoids is largely an untapped resource.
Does CBD help good bacteria?
Research in the past few years is beginning to indicate the ECS (endocannabinoid system) interacts and has certain control functions with gut flora (gut microbiota). Gut flora is an intricate community of trillions of microorganisms within the digestive tract.
The gut flora has three key roles:
- Defending against pathogens.
- Utilizing all available nutrients.
- Secreting chemicals to kill bad bacteria who seek to steal nutrients.
Infants are born without gut flora (good or bad bacteria) and we don’t have mature distinct healthy gut bacteria until we’re approximately 2.5 years old. At 2.5 years of age, approximately 300 – 500 bacterial species (2 million genes) exist forming a complex ecosystem. Humans have more gut bacteria than we do cells in our bodies and vastly more than the human genome (genetic material, aka DNA).
What species of gut flora will colonize is influenced by several factors. Some factors are mode of birth (vaginal or assisted), diet (breast milk or synthetic formula), sanitation levels, antibiotic exposure, and much more.
Humans are born with an ECS (endocannabinoid system) and its primary function is to regulate and control homeostatic balance between all systems within the body – potentially including regulating gut flora. Science suggests since human breast milk contains endocannabinoids, infants who breastfeed are likely to not have an endocannabinoid deficiency.
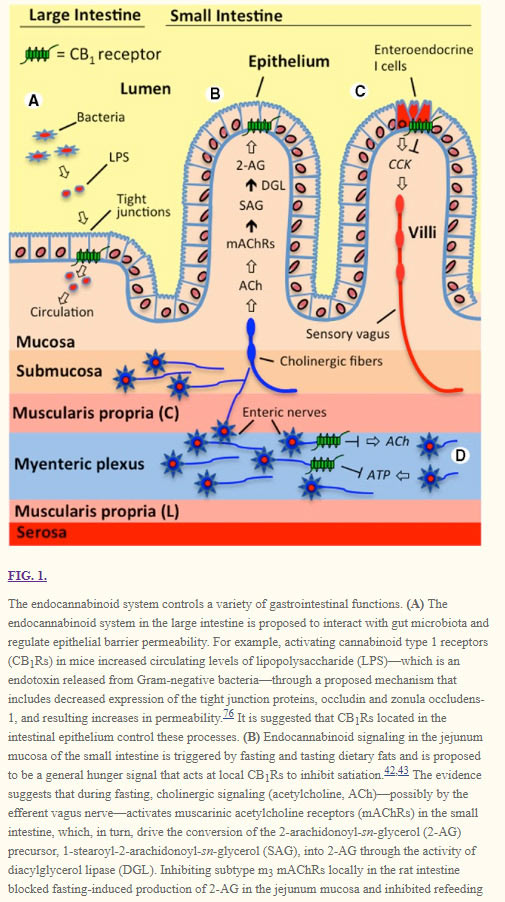
Photo credit: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4940133/
Research shows the existence of cannabinoid receptors in the ECS on the large and small intestines control processes that interact with gut bacteria.
Growing bodies of research are concluding single molecular compounds of fruits, vegetables, and other foods (such as hemp cannabinoids) are not where the health benefits come from. Health benefits are a result of the synergistic interactions between various bio-active nutrients in whole foods. The more variety of nutrients, the more health benefits are able to be extracted and used.
With a broad spectrum of phytocannabinoid nutrients, synergistic health benefits increase as the ECS receives essential nutrients. When the ECS (endocannabinoid system) has proper nutrients, it’s able to achieve a homeostatic balance between all systems within the human body.
We can infer since the ECS controls homeostasis (delicate balance between nearly every system in the body) – the ECS might also have some level of control in gut flora and regulating the homeostatic balance.
Broad-spectrum organic CBD oil has cannabinoids that help nourish the body’s ECS (endocannabinoid system).